I have never had an anaphylactic reaction to any drug. Anaphylaxis, according to what I have read, is actually quite common and can be life-threatening, so I understand the caution.
One of the most frustrating episodes a writer contends with is writer’s block. Wikipedia has a good definition of it, if you’d care to look. There is a link to it in the reference section at the bottom of this post. (1) Suffice it to say, sometimes it’s difficult to come up with something creative and new, and I am experiencing that condition at the moment. I want to update you on my doctor visit from yesterday and the status of the Darzalex infusions. It’s just hard to make the medical stuff very interesting, I think. I will do my best to keep you spellbound. Spellbound may be a smidgeon ambitious. I’ll settle for engaged.
It is always surprising to me to learn that someone has a different perspective than my own on my behavior and reactions to this condition I have, Multiple Myeloma. John accompanies me on nearly every doctor visit with Dr. Joudeh, and although he tends to be quiet and reserved around other people, he will often contribute his viewpoint during our visits. When we met with Dr. Joudeh yesterday, as always, I was prepared with several questions for him, but I always try to wait until he has shared everything he has with me first. He always covers my lab results, and yesterday’s were good. He also explained about the Daratumumab (Darzalex) change and the decision to pause it. It was primarily due to the first reaction when my tongue felt a little thick. I have never had an anaphylactic reaction to any drug. Anaphylactic shock, according to what I have read, is actually quite common and can be life-threatening, so I understand the caution. We will resume the Darzalex this Friday once again with a two-part infusion. The session will likely take several hours.
In the meantime, I have an appointment this afternoon at Eglin Air Force Base Hospital to see a doctor who will do the placement of a mediport to make the management of the Darzalex and all the other infusions a little easier.
That reminds me – I wonder if they’ll use the port to deliver the Velcade, the chemo that is injected into a fatty area, in my case my belly, so that it is absorbed more slowly. I don’t know if they will continue those injections or deliver the Velcade through the port. It’s not a big deal one way or the other. The injections don’t generally hurt; they’re just a little uncomfortable. I’m sure I will find out on Friday.
The timing of the port placement is a little tricky. It will have to be done in between my infusions, and I have 9 upcoming visits for lab work, infusions, and to see Dr. Joudeh. The really big question is when the bone marrow transplant will take place. My brain has been tentatively prepared for it to be in May for a while now, but it will depend on how I respond to the Darzalex.
When I looked back on the post “The Awaited Word,” I realized that Dr. Joudeh had since clarified the abnormal plasma number from my 25 February bone marrow biopsy. It was actually 12.2%, slightly higher than what I had thought. Our aim with the Darzalex, Velcade, and dexamethasone is to get that number around 5%. Please pray that happens in short order.
Dr. Joudeh entered the exam room yesterday, and for a few seconds, I think he wondered if he was in the right room.
“You have a new hairstyle,” he said.
“Yes, I thought I would simplify my life a little bit,” I responded. “It’s shorter than yours!”
He responded that it looked very nice as he sat down at the desk to cover my labs, answer my questions, and do a brief physical exam. We discussed everything I’ve mentioned thus far, and then he paused to allow me to ask my questions.
On my 12 March lab results as well as the ones from yesterday, my neutrophil percentage was 72.7. There was a comment included that read, “Possible left shift.” I had googled information about the neutrophils and what a “left shift” meant, and Dr. Joudeh confirmed what I had read. It could indicate that an infection existed or was possible. Of course, this was a concern for me, but Dr. Joudeh reassured me that the percentage was nothing to worry about and only a very slight change. He did not think it was significant.
The most pronounced side effect has been feeling intoxicated or as though I’m on speed or something. It’s really quite unsettling.
I also asked him about the side effects I have been experiencing. John suddenly piped up.
“She’s moody, she’s tired, she's grouchy…stressed out...” he trailed off.
He’s absolutely right. I would actually describe me as a total spaz. I’m amazed that he’s had the patience to tolerate me.
The most pronounced side effect has been feeling intoxicated or as though I’m on speed or something. It’s really quite unsettling. On two occasions within this past week, I have felt unsteady on my feet, unsteady to the point that I would most certainly fail a field sobriety test. And the chattiness! It’s hard to describe how I felt. I believe I told someone in a text message that I felt frenzied, as though I were running in fast-forward mode. It was kind of amusing but disconcerting to me at the same time. Thankfully, the effects lasted only a short time, maybe an hour or two at the most.
I told him the worst side effect, however, was the aching pain in my hamstrings and calves. It was almost unbearable. If you have ever started an exercise program that stretched these muscles in your legs, you probably felt the intense aching for several days after until you were able to work it out, right? That’s how it felt. Nothing helped. Not ibuprofen or acetaminophen or even my prescription of Tramadol. I was convinced it was the Darzalex.
“The intoxicating symptoms you felt are a result of the Gabapentin,” Dr. Joudeh told me.
We had increased the dose in the hopes that it would better alleviate the neuropathy I am experiencing in my feet and hands. The numbness and tingling, which can become permanent, are a side effect of the chemotherapy, and the Gabapentin helps relieve that side effect. It has been working, but now that I know it’s responsible for the frenzied feeling and unsteadiness, I will definitely be very careful about driving any distances.
If anyone reading this is a Star Trek fan, like I am, you’ll understand this reference. When I first picked up my prescription for Gabapentin, I immediately associated it with the Klingon dilithium mines on the penal asteroid of Rura Penthe, pronounced “ru·ra·PEN·tay,” to help me remember the name Gabapentin, “gab·a·PEN·tin.” I know it’s silly, but it worked for me. Rura Penthe is a reference from the movie “Star Trek VI: The Undiscovered Country.” I have included a YouTube clip that is kind of long, so if you fast forward to the 7:35 mark, you can hear the Klingon ruler sentence Kirk and McCoy to life on the penal asteroid of Rura Penthe. (2)
Dr. Joudeh went on to explain that the aching in my legs was due, not to the chemotherapy, but to the Zometa, the drug that I get once a month in a 30-minute intravenous session. It is given along with cancer chemotherapy to treat bone problems that may occur with multiple myeloma and other types of cancer (such as breast, lung) that have spread to the bones. (3)
“We may go to every three months on the Zometa,” Dr. Joudeh said, and that’s fine with me if it will ease that awful pain even a little.
As for the moodiness, fatigue, and grouchiness, I am trying to be more mindful of how I react to things. It’s so easy to lose patience quickly, especially with the ones you love the most, and they are the least deserving of such behavior. For me, the near-screeching responses that burst forth from my lips are so spontaneous, it’s difficult to filter them at all. John reassured me just this morning that he knows why I do it, and that makes it more tolerable, but he may retreat to his house more often if they continue. Who can blame him? I mean, one can only take so much.
I am reminded of another favorite scripture from Colossians 4:6:

**UPDATE**
It is Wednesday evening now, and I have been to Eglin Air Force Base Hospital to meet with Dr. Christopher Mahoney, the surgeon who will place my mediport on 2 April. He was very thorough and even used a demo mediport to show me precisely what the device looks like and each step as to how he places it under my skin near my collar bone. His favorite modifier is “exquisite.” He only used it a few times, but it’s such a unique word that one seldom hears, and me being a “word girl,” it definitely caught my attention. I liked him and felt comfortable with him.
When I texted Kohlson, who is back in the States at Fort Campbell, Kentucky (Yea!!), he wrote, “That sounds so painful.”
“It’s not,” I told him. “It helps things to be less painful,” to which he replied, “Well that’s good then I’m glad.”
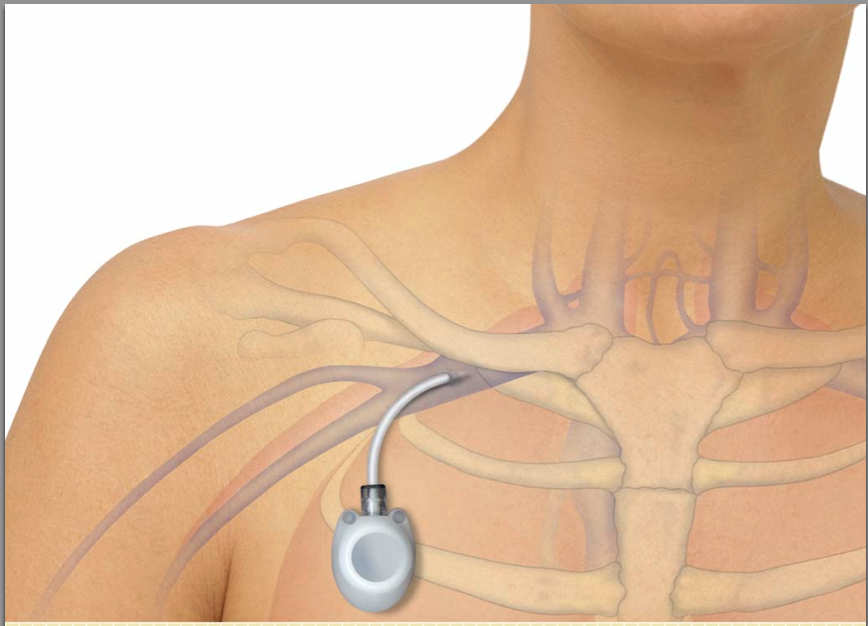
If you could see the ugly bruise on my arm from last week’s IV, you too would understand the benefit of the port. It eliminates needle-sticks to my arms that can weaken and even damage my veins over time. Don’t get me wrong – it gives me the heebie-jeebies to think about having a solid plastic or metal device implanted under my skin. It will leave a small bump where the port is placed, but the tube or catheter that goes into my vein will be invisible. I touched one today, and it is soft and pliable.

If you recall, in a previous post I mentioned the CVC, or central venous catheter, that Dr. Selby indicated they would place once I am ready for the bone marrow or stem cell transplant. Dr. Mahoney explained the differences between a CVC and a mediport and assured me that I could have both at the same time. The primary difference is the temporary nature of a CVC. A mediport can remain under the skin pretty much indefinitely and is comparatively maintenance free, but a CVC isn’t meant to be permanent and must be flushed every seven days in order to avoid the likelihood of infection. Along with the lovely graphics, I’ve also included a link to an interesting article that compares the two, if you’d like to read more about it. (4)
Like everything else involving this condition, I’m eager to get the procedure to place the mediport over with and move on.
I’m sure I’m leaving something out, but I am weary and need to hit the sack. Goodnight, dear family and friends. God bless you.

References:
(1) Wikipedia Contributors. 2021. “Writer’s Block.” Wikipedia. Wikimedia Foundation. March 18, 2021. https://en.wikipedia.org/wiki/Writer%27s_block.
(2) These Are the Voyages. 2016. “Star Trek vi the Undiscovered Country - Klingon Justice.” YouTube. https://www.youtube.com/watch?v=K5StGrDJU5w.
(3) Marshall, BPharm, MRPharmS, Helen. 2020. “Zometa: Side Effects, Dosage, Cost, Uses, and More.” Www.medicalnewstoday.com. October 21, 2020. https://www.medicalnewstoday.com/articles/zometa.
(4) Fauntleroy, Glenda. 2019. “Central Venous Catheters.” Healthline. August 29, 2019. https://www.healthline.com/health/breast-cancer-navigator/central-venous-catheters-picc-lines-versus-ports.

It’s sounds like you have a wonderful caring group of Doctors! I’m glad John goes to your appointments with you, it helps having someone else to hear what the doctors are sayin, AND speaking up telling the doctors how you really are. I loved how he just said how it is! Lol Hope to see you soon! ❤️